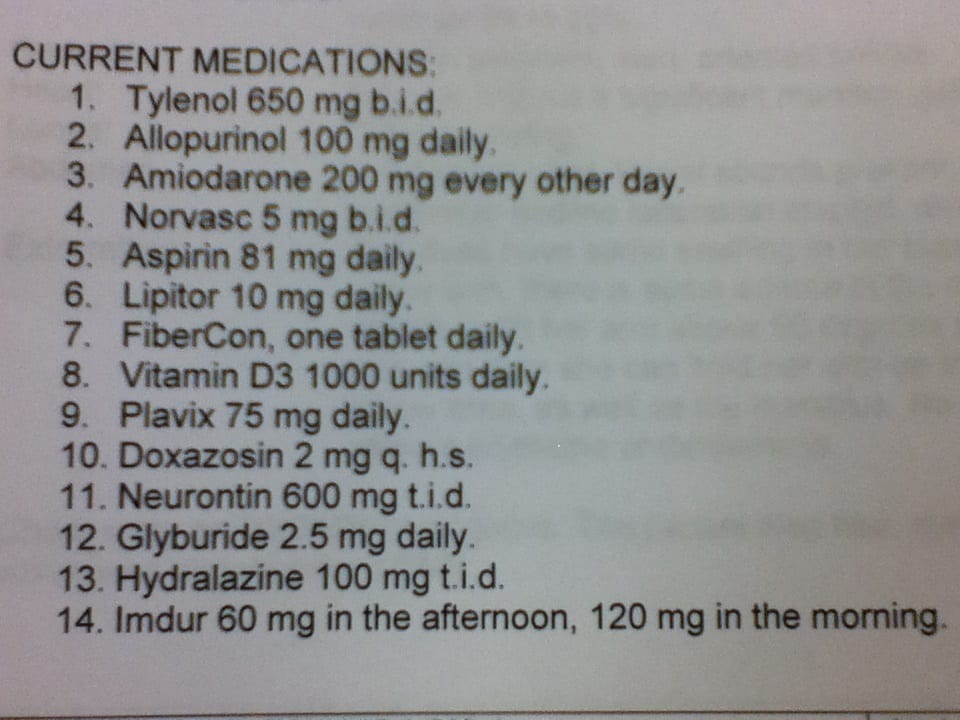
Let’s do a med list review, it’s been a while… Remember with these cases, I really try to highlight the most important things I want you to think about. There are multiple things to monitor in these case reviews, as well as multiple patient specific factors that can really effect the way you prioritize your items to address.
Some thoughts:
Hydralazine and Imdur doses are pretty substantial, leading me to believe that this individual has significant cardiac/hypertension issues. Also on amiodarone, Norvasc, Aspirin, Plavix, Lipitor, doxazosin. Blood pressure monitoring will be very important. Remember that Amiodarone has some funky side effects to monitor for.
Appears they have diabetes with the glyburide Rx. I’d investigate why they aren’t on an ACE or ARB especially since they most likely have significant issues with blood pressure. If they haven’t been on an ACE or ARB for some odd reason(allergy or ADR), I’d maybe look at a transition from the doxazosin, unless using doxazosin for BPH/HTN.
Some pain issues with scheduled Tylenol (and likely gabapentin at a decent sized dose), and would suspect gout with allopurinol Rx.
I’d try to investigate why Norvasc is BID – but some providers prefer twice daily especially if having variable BP’s
Sound off if you’ve got something to add!
Thanks for reading! I’m giving away a 6 page PDF on 30 medication mistakes I see in my practice, please take advantage of the free and unique opportunity!



Using the Norvasc as a case in point in many cases pharmacist will refer to their computer data base or lexicomp etc. and jump at “they should be taking this once a day, it says so —–” We often forget that its the patient not the drug we are treating and patients will respond to high and/or low doses and will take medication which are more commonly dosed twice a day only once and vice versa. Its the outcome and a patients response that counts not whatever the PDR may say.
Always important to investigate why patients are taking meds the way they are!
Definitely a cardiac patient. Heavy doses of heart and blood pressure and pain. Very low dose on Lipitor makes little sense. Fibercon one a day no effect with these drugs. Lots of constipation.
I wonder how dizzy and sluggish patient is?
Is this a post-MI or post-stroke patient?
How long have they been on Plavix + ASA, are both still indicated?
Is Amiodarone being taken for A Fib? If so, does CHADS2 score add up to indicate to use an anticoagulant?
For the diabetes, they’re on Glyburide but not Metformin. Do they have renal imairpment and afraid of lactic acidosis with metformin? And why glyburide which has high liklihood of hypoglycemia vs. Gliclizide (long acting)?
Why given amlodipine bid…but should be give at.once 5 or 10mg
And amiodarone why in every other day not daily?
Why is the pt on glyburide when there are so many better diabetic meds today. Last conference I went to, the speaker ( physician) asked the physicians in the audience as to who still has their pts on glyburide. Her suggestion was to switch them. Metformin is much better choice to start, if the pt does not have renal issues.. The SGLT2 are promising and data is showing CV death reduction with empagliflozin.( 32% decrease in all cause mortality)
Wonder about amiodarone 200mg every second day. Why not 100mg every day? This drug is a falls risk.
Acetaminophen dosing is strange. Need to ask questions about pts pain. Perhaps acetaminophen 650mg qid would be more useful. As well, is pts pain managed with Gabapentin? Is pt having sedation, side effects with gaba? Perhaps pregabalin may be a better choice? Where is the pain? Perhaps voltaren cream may be useful as well?
What about the 12 hour nitrate washout period that appears to be overlooked for a twice daily dosing of Imdur.
I’m new here, and just studying for my CGP exam, so feedback is greatly appreciated! I’m assuming this patient has heart failure and was treatment resistant to ace Inhibitors – which would explain the use of hydralazine and ISDN (based on V-HeFTII). The doses of hydralazine and ISDN are high, but still within range for HF and I see no issue with the twice daily dosage of ISDN since the doses are morning and afternoon (i.e. 8am and 2pm is preferred, right?) So, my first concern with the med list is the use of doxazosin in a HF patient (or at minimum in a patient with chronic hypertension). Based on ALLHAT, doxazosin was shown to increase the risk of CHF compared to chlorthalidone- and recommendation to stop use of all alpha-blockers was made for since treatment of HTN should increase your risk further of CHF. Additionally, if the patient does have HF, wouldn’t a beta-blocker like metoprolol/carvedilol be a better option than amlodipine? With no diuretic on board I assume the patient is not having fluid retention, but that would be something to check. Since the patient also has gout, I would research if/what the prior failure to ACE/ARB was…losartan is helpful in increasing uric acid excretion and could potentially lead to stopping allopurinol (along with cardiac benefits).
It appears the patient would have a CHADS2 score of 3+ which should be treated by an OAC, so I would determine the bleeding risk to determine if an OAC is safe.
As for the amiodarone dose, I see nothing wrong with it- 200mg qod is a preferred dose to minimize toxicity and the long half-life (especially after chronic dosing and in elderly with higher fat %) allows for qod dosing.
Lipitor dose is on the low side, especially based on risk factor…however, it is most likely due to drug interaction with amiodarone or tolerability. I would consider changing to rosuvastatin 20mg and adjust downward based on tolerability.
The glyburide is typically a poor choice due to long half-life in elderly, especially with amiodarone which is a 2C9 Inhibitor. Metformin is the obvious first choice and I wonder if either GI ADRs were intolerable or kidney function is limiting use. If poor renal function, then a sulfonylurea or SGLT2 inh cannot be used either, and a TZD is a poor choice in HF. I would then start the patient either on Januvia 25mg or basal insulin, depending on patient preference- or try and ER version of metformin and administer with food if the GI issues were the problem.
Feedback? Thanks!
I forgot to address the doxazosin…I assume the patient has BPH as I don’t see any psych meds to suggest otherwise…aside from previously mentioned concerns with worsening HF, it also causes orthostatic hypotension. Obviously a PDE Inhibitor is out as it is contraindicated with ISDN. There is some data showing carvedilol may be helpful in BPH symptoms, so that would be my first approach. This would target the HF component and BPH. If, however, carvedilol isn’t suitable, finasteride is safe in renal insufficiency and has antiandrogenic properties which may benefit a HF patient.