Looking over this medication list, there’s plenty of stuff to pick on, I’m going to limit myself to two things to further investigate and let you all help with the rest. Feel free to speculate on diagnosis, appropriate alternatives, potential causes of polypharmacy etc.
Always important to take a look at the Lovenox (enoxaparin) dose and make sure it is correct and that we have an end date in mind when using for prophylaxis. I’m also going to look at the Indocin (indomethacin) with the Lovenox as this patient will be at high risk for GI bleeding. They are on Aspirin as well. GI protection should be considered with close monitoring of hemoglobin/platelets while on the Lovenox especially.
So many to choose from, but that Seroquel just screams at me as I’ve seen antipsychotics used so many times for acute delirium type situations and then left on board long term. I’m going to try to investigate why this patient was put on this medication and see if we can’t get possibly get rid of it. With the use of thiamine, this patient could very well have a history of alcoholism, something to dig into as well in the patient history.
Thanks so much for reading this content – if you enjoy this, I’d like to give you access to a free webinar on polypharmacy! I created the webinar based on my real life experiences as a clinical pharmacist – please Click Here to check it out!


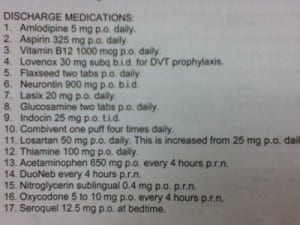

That’s a high dose of APAP, I’d be concerned of hitting the 3-4gm/dy.
Also: both DuoNeb AND Combivent? same drugs in both products (and Facts & Comparisons says DuoNeb is discontinued?)
don’t know patient age but probably needs a statin
Also, is this post-MI? probably switch amlodipine to a beta-blocker
Thanks for the comment!
Without diagnoses it’s virtually impossible to make intelligent comments about what might be wrong – or right – re: this patient’s meds.
Unless the patient has alcoholic cirrhosis , I’m not concerned about the APAP – maybe just change it to q6hprn.
Not every old patient needs a statin… Let’s look at a lipid profile and make an appropriate decision, which may not be a statin. And, flaxseed may not be needed either; perhaps OTC USP-approved fish-oil caps – not Lovaza, the biggest rip-off to get by the FDA lately.
With unknown diagnoses, it’s impossible to recommend a beta-blocker over amlodipine.
What dose of glucosamine are they on? At any dose, the efficacy of the drug is debatable.
And without diagnoses, it’s a crapshoot re: other meds as well.
Why are they on high dose B-12 and B-1? Innocuous drugs, so I’m not too worried.
Why are you so worried about low-dose Seroquel? I had a 67-year-old patient taking 300mg qHS with no AEs except perhaps a little weight gain, which may have been good.
Why are they on Oxycodone? And doesn’t current law require a specific dose – not a range of doses? A nurse cannot make dose decisions.
Why are they on Neurontin? 600mg TID would likely be better than 900mg BID, if it’s needed.
Probably the ASA could be cut to chewable baby aspirin 81 mg/day, rather than 325mg/day of a solid tablet – two factors that can increase GI bleeds, especially with indomethacin being used.
Why is indomethacin being used? If an NSAID is needed, consider the much safer diflunisal.
More concerns come to mind, but, again, without diagnoses…
Thanks for the comment! What I’m looking to try to educate folks on is the thought process not the answer. I think colleges/schools don’t adequately prepare young professionals how to think things through and prioritize. I think the med lists provide a great discussion tool to provide critical thought versus a correct answer. Not only that, continuously learning healthcare professionals get to see high quality healthcare professionals like yourself “think out loud”! I do concur that the Seroquel at that dose will likely be tolerated, but I’ve seen those baby doses used numerous times for acute delirium type situations and just kind of get left hanging out there even when the delirium resolves, contributing to polypharmacy. Simply speculating based on a few of the things I’ve seen. Thanks again for your contribution! If you’d like to contribute a case or help improve medication education, please let me know! – Eric
My thinking, with regards to the statin, is that according to the 2013 ACC/AHA lipids guidelines, actual lipid values are not as necessary as previous because of the identified 4 major statin benefit groups. The prescription for nitrostat makes me think this patient is post-mi, acs, or has angina, which is part of the first benefit group: “clinical ASCVD” which indicates they should be on a statin. While I agree about the flaxseed oil, given its lack of bioavailability in humans, there are 2 reasons I didn’t suggest changing anything about it. First, in my experience, people take supplements because they think they work and only under rare circumstances (like if you can well-document risk of harm) will they stop them just because you tell them too. They think they’re harmless. Second, the lipid guidelines I mentioned above discourages the use of any non-statin cholesterol drugs due to the lack of mortality benefit. So I wouldn’t bother recommending changing flax for fish.
With regard to my suggestion to switch amlodipine to a beta-blocker, that was contingent on whether or not this patient truly *is* post-mi, like I’m purely guessing is the case, the 2012 ACCF/AHA STEMI guidelines say that a BB is preferred over a CCB because a BB has proven mortality benefit and a CCB might actually be detrimental. But, like you said, its hard to make firm recommendations with a lack of diagnoses
Well, the guidelines may not recommend fish oil, but there are plenty of studies that suggest benefit beyond cholesterol lowering so this may be an example of a time where the guidelines are a starting point of recommending what’s best for your patient.
Thanks for the comment Jen!
If the pt is on nitro SL prn, he/she should be on a statin as long as there is no significant intolerance… regardless of the lipid panel. Refer to 2013 AHA guideline update. I do agree that a lot is unknown without knowing PMH, lab results, etc… but a retail pharmacist could make this intervention with some discussion with the pt.
This reminds me of my hospital rotations in psychiatry! This is awesome!
First, this Rx profile screams of an elderly person who suffers from moderate to severe osteoarthritis ( or a poorly managed rheumatoid arthritis patient since no DMARDs) and was admitted for DVT (as stated) requiring anticoagulation. This patient probably has either primary hypertension with a history of chronic stable angina ( this would explains NTG, multiple antihypertensives ) along with fluid retention possibly to normal decrease of renal fx due to old age ( furosemide ). The patient might also suffer from either post-herpetic neuralgia or epilepsy ( gabapentin). Dose should be adjusted according to Creat clearance and divided T-QID… This patient must be somnolent with gaba/oxycodone/seroquel combo…
Like others have suggested, we would need to clarifie diagnosis and compelling indications for CCB over beta-blockers, why no statin (primary or secondary prevention?)… Discontinue glucosamine ( evidence is mostly negative, see GAIT trials), flaxseed and vitamins unless clear indication.
I agree that most pressing issue is risk of bleeding and that should be resolved ASAP ( discontinue indomethacin if possible and start with longacting analgesic like long-acting tramadol, if indicated and PPI…)
I also would question with respect to bleeding risk the Flax Seed. FlaxSeed slows clotting. I would attempt to find out why he is taking it. Is it for constipation possibly due to Oxycodone or other purpose? Perhaps a stool softner would be a better choice.
Your informations should be followed by physician also
Be careful with tramadol in the elderly risk for serotonin syndrom, seizures, confusion, and possibly hypoglycemia.
other than diflunisal, what nsaid would you safely recommend with lovenox?