Another Guest Post via Amanuel T. B.Sc., Pharm.D. – Clinical Pharmacist: View his profile on Linked In
Have a passion for medication education? Would you like to give back to healthcare students? Would you like to be an expert on a particular topic and increase the size of your professional network? Please be a guest contributor and donate a medication related case that all healthcare professionals can learn from!
Thanks again to Amanuel for his dedication to medication education and donating his time and talents!
If you haven’t subscribed yet for future updates and access to more free clinical medication content, please Click Here to do so!
A 76 year old woman with a history of heart failure and s/p mitral valve repair asked to get a medication for her back pain. She specifically requested to be on Ibuprofen (NSAID) 600mg, a regimen she claimed (and documented on her chart) was getting as an outpatient with good results.
A pharmacist was consulted for advise on whether or not it’s appropriate for patient to be on this analgesic drug.
Upon review of her medical chart it was revealed that patient was on antiplateletes: Clopidegrel 75mg and Aspirin 81mg for heart failure and lisinopril 5mg. Lab review showed a remarkable decrease in platelet count from 207k to 143k in a 36 hour period. Heparin Induced Thrombocytopenia (HIT) was ruled out for patient was not receiving heparins or any other parenteral anticoagulants that are associated with HIT during her admission.
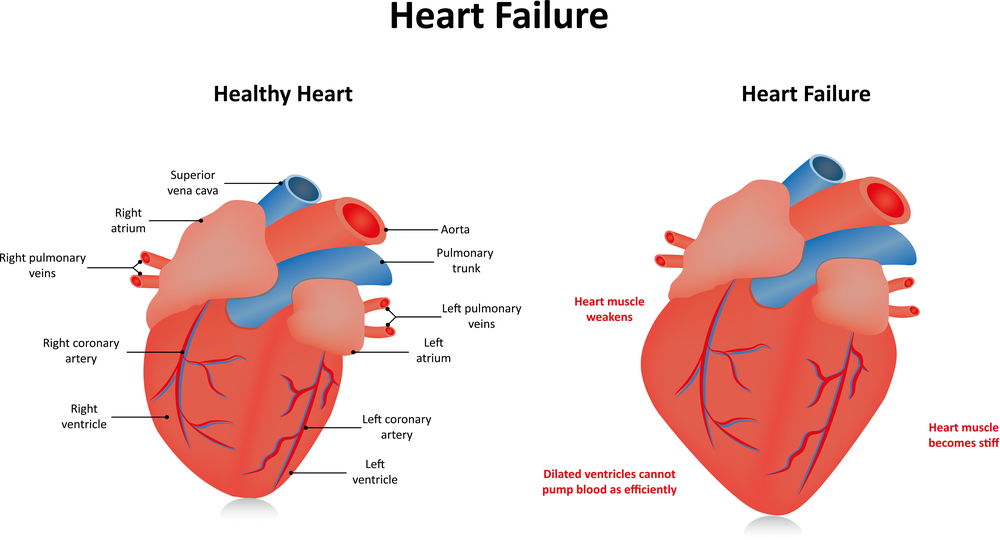
Patient was experiencing fluid retention associated with the heart failure and complained of swelling of her upper extremety.
Ibuprofen is a NonSteroidal Antiinflammatory Agent that’s widely used as an analgesic and in treating various types of inflammations including rheumatiod arthritis and osteoarthritis. However, there are several factors which preclude this patient from having this drug as part of her regimen: Ibuprofen inhibits platelet aggregation ; thus adding another antiplatlet agent to the regimen she is already on will certainly put her at increased risk for bleeding. This is specially true given that patient’s platelet count has dropped significantly in a short period of time. Fuid retention and peripheral edema have been reported with a chronic use of Ibuprofen and should be avoided, if at all possible. Also note that the patient is on Lisinopril-an ACE Inhibitor- for hypertension. There is a documented risk for renal toxicity and injury when Ibuprofen and ACE Inhibitors are used concomitantly. Ibuprofen has also been associated with decreased renal blood flow via inhibition of prostaglandin.
Given the patient’s medical and medication history and the drug-drug interactions with other drugs, use of Ibuporfen should be totally avoided.
There are a number of other analgesics that could be recommended as an alternative to Ibuprofen. Tramadol HCL in a smaller dose has been shown to be as effective as and with less adverse effects when compared with Ibuprofen , especially in patients with heart failure. Naroctic analgesics such as oxycodone or oxycodone/acetaminophen, in small doses and short term, could be considered if patient has no response to or is intolerant to Tramadol. Risk of fall, respiratory depression are common occurrences associated with narcotic analgesics and as such should not be used routingly.
The Pharmacist, after reviewing patient’s med history, made his recommendation to discontinue Ibuprofen and place her on Tramadol 50mg given q6-8 hours prn pain.
For updates and access to premium content, please subscribe on the right hand side of the page (or bottom for mobile users) if you haven’t already done so! An email address is all that is necessary and we respect your email privacy.


Nice! Helpful!
Glad you find the piece helpful and thanks for the comment.
very helpful.. most of my patients/customers rely on the ibuprofen 200mg..my usual concern and recommendation are geared towards preventing GI upsets so thanks for reminding me to look yet closer. .
The patient described needs 4000mg of omega3 daily for all her problems: pain, inflammation, platelet aggregation, edema, hypertension. Consume 2 tablespoons of ground flax seeds to get 4000mg of omega3. Mix in food or wet with organic coconut oil, add some plain cacao powder to make chocolate pudding. The lady needs to eat vegan. She would also do better if she takes #VitaminD 10,000 units daily until her blood level increases to about 75ng/ml. She should consume more magnesium than calcium. She probably supplements with calcium but not with magnesium; calcium increases muscle rigidity while magnesium will relax those back muscles and sciatic nerves.. Vegetables, nuts, seeds, avocado will supply magnesium.
Thanks for providing the alternatives….
I find Tramadol has lots of drug interactions and it should be used with caution in the elderly because it may cause dizziness and reduce the seizure threshold.
I do agree with Ravinder +++
I would give acetaminophen 500mg q6h first.
I’m also concerned by your message on the antiplatelet effect. Actually, it has been show in vitro that ibuprofene interacts with AAS and can block the beneficial antiplatelet effects.
https://www.ncbi.nlm.nih.gov/m/pubmed/28293429/
Agree.