by Eric Christianson | Jan 21, 2026 | Polypharmacy Cases And The Prescribing Cascade
One of the biggest contributors to polypharmacy isn’t the number of diagnoses a patient has—it’s our mindset around medications that fail to deliver benefit. Everyone knows we need to reduce meds in geriatrics, but how do we do that? Too often, when a drug doesn’t...

by Eric Christianson | Jan 7, 2026 | Polypharmacy Cases And The Prescribing Cascade
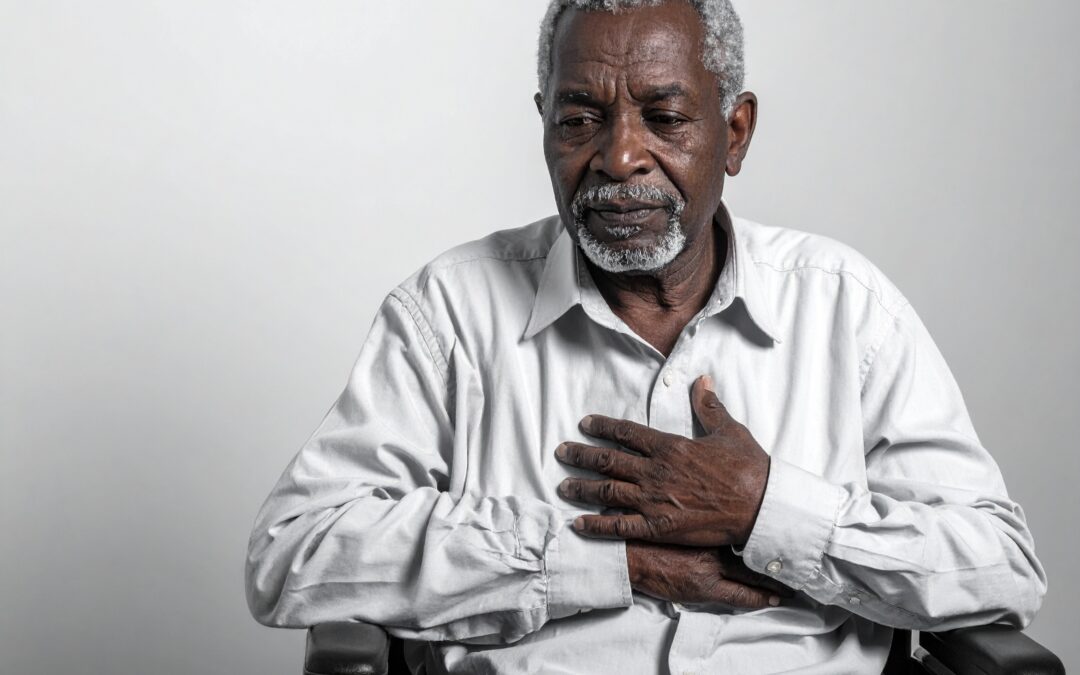
Mr. H is a 78-year-old male presenting to a primary care clinic for a routine medication review. In this scenario, we want to identify deprescribing targets. His past medical history includes hypertension, heart failure with preserved ejection fraction (HFpEF),...

by Eric Christianson | Oct 1, 2025 | Polypharmacy Cases And The Prescribing Cascade
I was asked a question the other day about trying to reduce medications in a patient on hospice. More specifically, how to address the use of PPIs. Proton pump inhibitors (PPIs) are some of the most overused medications we see in clinical practice, but hospice...

by Eric Christianson | Sep 7, 2025 | Polypharmacy Cases And The Prescribing Cascade
In this case scenario with gabapentin and metolazone, I lay out how the prescribing cascade can rear its ugly head. SK is a 74-year-old male with a past medical history significant for chronic kidney disease stage 3, type 2 diabetes, hypertension, peripheral...

by Eric Christianson | Aug 10, 2025 | Polypharmacy Cases And The Prescribing Cascade
Mrs. M is an 87-year-old female residing in a skilled nursing facility. Her medication list includes: Apixaban 5 mg BID (for atrial fibrillation) Docusate 100 mg BID Senna 8.6 mg BID PEG 17 g daily Calcium carbonate 500 mg TID Lisinopril 10 mg daily Metoprolol...

by Eric Christianson | Aug 6, 2025 | Polypharmacy Cases And The Prescribing Cascade
Here’s a question that comes up in hospice more than you’d think: Why would a hospice patient be on two antipsychotics at the same time? To the average clinician, this raises immediate concerns—duplication, unnecessary side effects, and polypharmacy in a population...